Let me start with two disclaimers:
1. I am grateful we have antidepressant medications. I have a long clinical career of using them and understanding when they can be lifesavers. When I do use these medications, I always underscore that they aren’t usually enough, they give us the capacity to do the other work necessary for our mental health as well. I also have many people coming to me wanting to wean off of them because of side effects. I support tapering if it’s safe and wise for their situation.
2. As well, if you are presently living through very challenging times in your life or the world, and have relied on an anti-depressant as one of your mental health tools, now may not be the time get off this medication. I always work with patients to decide when their internal and external resources (community, therapy, access to movement and good food, etc) are plentiful. But if and when you decide to do so, always do it under medical supervision and please read the article below.👇🏽
I am embarrassed to say that I was well into my career as an Integrative Family Physician before I truly understood how to taper anti-depressant medications.
💡In residency training, I was taught to wean them slowly (that was wise) but not taught how slow was slow enough to do this well and gently for the patient.
💡In residency training, I was taught to be cautious about relapse with a taper (that is wise) but I was not taught that relapse could be easily confused with withdrawal and that I may be restarting a medication that is not needed.
💡And maybe most importantly, in residency training, I was taught to go more slowly at first and that once we got to lower doses and patients were doing okay, it was safe to go off the medications. (not wise)
These are some truths to start off with:
When anti-depressants work, they improve symptoms by on average 30%. This can be life-saving literally but is for most people, not enough, to feel like they are living the vibrant, thriving life they desire.
Anti-depressant medications are one of the most commonly prescribed medications in the UK and US and in the US, nearly half of individuals using these medications have been on them for more than 5 years.1
They come with a host of side effects that are well-documented and troubling to many patients, such as GI disturbances (which makes sense if you remember that 60-70% of your serotonin is made in your gut), sexual dysfunction like decreased libido or anorgasmia (both very distressing to someone’s life and mental health), and weight gain (again, very distressing to mental health) to name a few. The other complaint that lands patients most often in my office asking for a taper is this general sense of feeling numb, that feeling down is more mitigated on the medication but there is also a sense that so are any ups. In essence, they feel less of anything.
The teaching (as I mentioned above) and guidelines on how to taper these medications are wildly out of date with the scientific literature. Although the American Psychiatry Associations’s guidelines2 (not updated since 2010) speak to the counsel of going slowly, they refer to this being over several weeks (which is not individualized to the amount of time the patient has been on the medication and in general, in my clinical experience, is too short) and they do warn of risk of relapse but do not give any counsel on how this could be differentiated from withdrawal.
👉🏽 So what do you need to know if you or your loved one have been on an anti-depressant/anti-anxiety medication for years and you are hoping to taper off the medication with medical supervision? (PLEASE always do this under supervision)
The brain adapts to long-term use of anti-depressant medications
What this means in practical terms for you is that stopping them can cause a withdrawal reaction. Your brain is used to having them, this is a physical dependence that is distinct from an addiction. And when they are taken away, the brain needs time to adapt to having less of them.
The symptoms of withdrawal are based on the time the changes in the brain take to resolve, not the amount of time the medication has been out of the system.
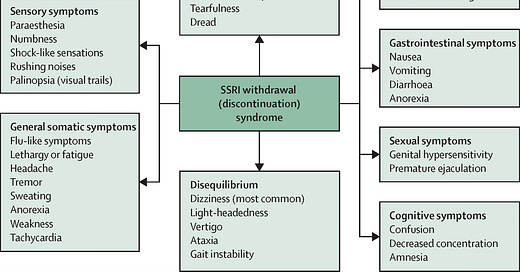
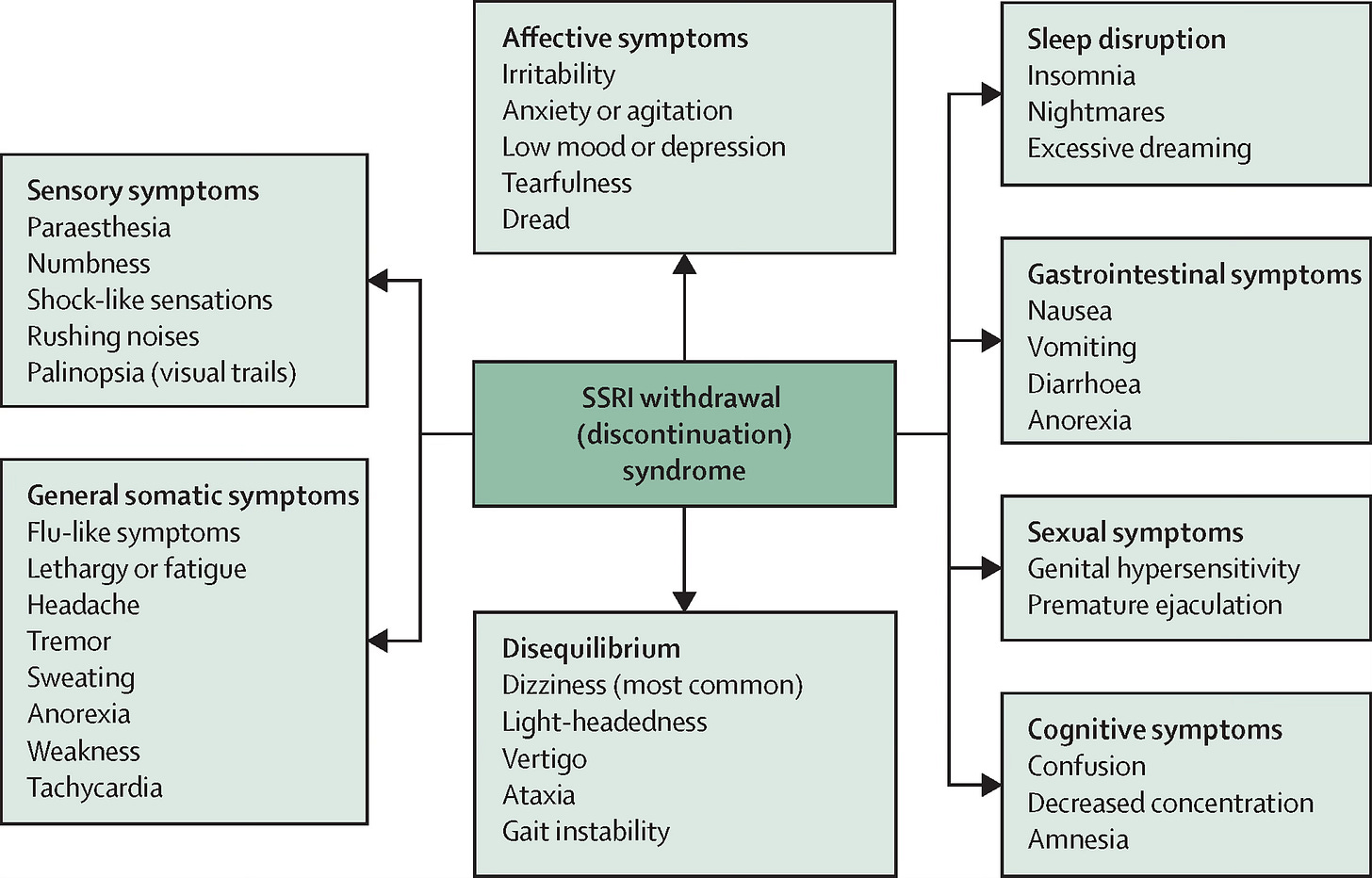
The symptoms can be both physical and psychological and have a wide range. The list is extensive as you can see below.
In double blind Randomized controlled trials, about half of individuals can have some or more of these symptoms and about half categorize them as severe.3
Of course, in general, the higher the dose or longer a patient has been on the medication, the more chance of withdrawal symptoms.
Withdrawal can be easily confused with relapse.
You can imagine how easy this is for patients and providers given that many of the psychological symptoms are the same as the original depression or anxiety that necessitated the medication to begin with. The key here is to realize that withdrawal is of quicker onset than relapse, it often has new symptoms previously not present and it rapidly resolves by increasing the dose of the tapered medication back to a dose where these symptoms were not present.
This was a common story I would experience. The patient would wean, even slowly it seemed, but when they felt anxious or depressed right away, it felt like it “wasn’t working” to taper.
Tapering needs to happen even more slowly as you get to lower doses.
This seems counterintuitive that lower dose reductions would be harder to tolerate but this is where the magic of understanding the brain physiology comes in. Dr. Mark Horowitz, based in the UK who by the way is an amazing source of knowledge on this topic and I credit him with making it so clear for physicians at large, showed in his study that doing a linear taper (i.e halving the dose repeatedly every 2-4 weeks) is not as effective as a hyperbolic taper where you cut the dose by a percentage as you go down.4 Let me explain.
If you are on 40 mg of citalopram, you and your doctor might be inclined to reduce it by 10 mg every 2-4 weeks as able. This seems reasonable. But tapering regimens with linear dose reductions will cause increasingly severe withdrawal reactions because of physiology that I will happily geek out about in the comments if anyone is interested. But the nutshell is that the serotonin receptors’ occupancy by the medications become increasingly large in an exponential way when you taper in a linear fashion.
In the following image borrowed from Dr. Horowitz, you can see that the magnitude of risk of withdrawal goes down when you do this kind of hyperbolic tapering at the lower doses where the brain has a harder time adapting to the loss of the medication.
So the answer is to go slower as you get lower. Very slow. In fact, studies show that patients who failed linear tapers can be successful on hyperbolic, slower tapers as shown by Groot and Os in their studies using tapering strips (these allow more fine tuned dose reductions vs tablets that are hard to cut) as seen in the image below.5
So, let’s put this all in practical take-aways for you as a patient who is discussing a possible taper with your doctor.
🩺 First, make sure this is the right time in life where you are well supported and feel ready for a taper, especially if you have been on the medication for years.
🩺 Know that feeling anxious/depressed can be common during withdrawal.
🩺 Try and work out a much longer taper with your physician that is over months or even longer if needed. Several weeks may not be enough.
🩺 Think about hyperbolic tapering or going very slow at the lower doses. It’s okay if you are on fractions of doses for the last parts of the taper. You want to do this slowly so your brain can adapt.
🩺 To do the very slow hyperbolic taper, you will need liquid versions of medication as tablets are hard to cut. Or your physician get tablets compounded at a compounding pharmacy. The main critical step is to go very slow as you get to those lower doses where your brain has a harder time adapting to not having the medication.
🩺 No matter how you taper, if you have any withdrawal symptoms that are uncomfortable, your doctor can always go back to the last dose where you did not experience them. Then you can go slower in the reduction from there the next time you try to taper.
🩺 If you have tried to taper before and not been successful, there is hope. It may not have been slow enough for you.
🩺 The real message is, go slow and know that is normal. Your brain has adapted to a medication and it takes time to adapt to not having it. Have an open conversation with your physician about this, I have yet to see a doctor who is not comfortable with tapering a medication more slowly.
And don’t forget, for paid subscribers, there is a workshop at the end of February (Saturday February 22nd at 10 AM PST/ 12 PM CST/ 1 PM EST-Zoom link in an upcoming email) for Heart Health Awareness Month. I will spend 20-30 minutes teaching you specific and practical evidence-based nutritional tips that you can implement easily and strategies to manage stress, both of which are essential for heart health. And then you’ll have time to ask questions as well. I’ll make it concise because I know you are busy! I always look forward to connecting with you deeper in these workshops.
Meet me in the comments as usual and let me know if you have any questions. Have you ever tried to taper a medication and found it difficult? You’ll find you aren’t alone in that experience. Are you thinking of tapering off an anti-depressant medication and found this helpful? As a side note, I said this at the beginning but it is worth saying it again—Do not taper any medication without your physician’s supervision and please if you are reeling from the situation in the United States right now and are on an anti-depressant/anxiety medication, do not feel guilt if now is not the time. You need all the tools that help you tolerate this stress. I’m with you in solidarity and will continue to empower this community with evidence-based health information and cut through the noise and misinformation out there. This is a time to lean on each other and those we trust, I am grateful to be in community with you.
Mojtabai, J of Clinical Psychiatry, 2014.
https://psychiatryonline.org/pb/assets/raw/sitewide/practice_guidelines/guidelines/mdd-guide.pdf
Davies, Addictive Behaviors, 2019.
Horowitz, Lancet Psychiatry, 2019.
Groot and Os, Ther Adv Pscyhoparm, 2021.





Horowitz has been a guest on several podcasts, kesser did a whole series on ssri tapering. Very informative.
Currently, I have tapered my with my provider's knowledge to 1/4 of my initial dose. However, when I have tried to go lower the sensory withdrawal symptoms described in the chart send me back to this level. I am going to try a slower hyperbolic approach as you described. Those shock type sensations with visual disturbance and vertigo are the worst. For me, it feels like a dog is shaking my brain like a toy.